SEO Summary:
- Even mild, chronic dehydration causes the body to release vasopressin, a hormone that constricts blood vessels, leading to elevated blood pressure.
- Dehydration also thickens the blood, forcing the heart to work harder, which further stresses the cardiovascular system.
- Achieving proper hydration requires balancing water intake with essential electrolytes (sodium, potassium, magnesium), not just plain water.
My Discovery: The Silent Link Between Thirst and Tension

I used to think of dehydration as something dramatic—extreme thirst or dry mouth after a long run. But I’ve since learned that chronic, mild dehydration is one of the most common and overlooked contributors to elevated blood pressure, quietly stressing the cardiovascular system every single day.
It was a revelation to me that simply being a little short on fluids could cause my blood pressure to creep up. The process is subtle, but the scientific mechanism is powerful: when your body senses even a small drop in fluid volume, it panics. It’s a primitive survival response that initiates a cascade of effects designed to conserve every drop of water—a cascade that inevitably includes constricting your blood vessels.
I want to walk you through this hidden connection and share the crucial advice I learned: drinking plain water alone isn’t always enough. To truly manage your blood pressure through hydration, you must understand the vital role of electrolytes in maintaining the delicate fluid balance your heart and arteries need to thrive.
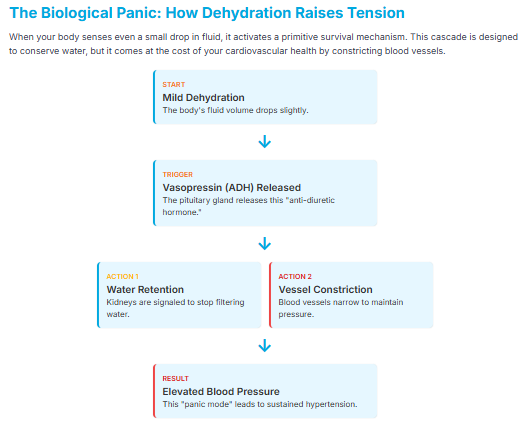
The Biological Panic: Vasopressin and Vessel Constriction
The moment your body registers dehydration—long before you consciously feel thirsty—it releases a hormone from the pituitary gland called vasopressin (also known as the anti-diuretic hormone, or ADH).
The Dual Action of Vasopressin
Vasopressin is your body’s water-saving command system, and it has two primary effects that directly impact blood pressure:
- Water Retention: It signals your kidneys to stop filtering water and retain as much fluid as possible.
- Vessel Constriction: To increase the volume of fluid relative to the size of your vessels (and therefore keep blood pressure from dropping too low), vasopressin causes the blood vessels throughout your body to constrict (narrow).
This vessel constriction immediately raises your blood pressure. Essentially, your body is trading optimal cardiovascular health for basic fluid preservation. If you are chronically under-hydrated, this mechanism is constantly at work, leading to sustained hypertension.
Additionally, when you’re dehydrated, your blood plasma volume decreases, causing your blood to become thicker and more viscous. This forces your heart to pump harder and faster to move the sluggish fluid through those newly constricted vessels, adding tremendous long-term stress to your heart muscle.
The Hydration Trap: Why Water Alone Can Be Worsening
When people realize they are dehydrated, the first solution is always to guzzle a large glass of plain water. While this is good, it can sometimes worsen the underlying problem if done excessively or without balance. This is the hydration trap.
The Electrolyte Dilution Effect

Your body needs a specific balance of electrolytes—minerals like sodium, potassium, and magnesium—to regulate fluid movement into your cells. If you drink massive amounts of plain water quickly, you dilute the electrolytes already in your system.
This dilution can lead to a state where your cells still aren’t effectively hydrated (because the osmotic balance is off), and you lose those crucial minerals through urination. These electrolytes are absolutely vital for managing blood pressure:
- Sodium: While high sodium is often blamed for hypertension, some sodium is essential for fluid balance.
- Potassium: This mineral helps relax blood vessel walls and promotes the excretion of excess sodium.
- Magnesium: Acts as a natural calcium channel blocker, helping blood vessels relax.
The key to healing blood pressure through hydration is to ensure you are replenishing both water and electrolytes.
My Protocol for Achieving Optimal Hydration Balance
I learned that true hydration is a dance between water and minerals, which is why individual needs vary so widely based on activity level, climate, and diet.
1. Don’t Just Chug—Sip and Space
Instead of drinking huge quantities of water all at once (which leads to quick urination and electrolyte flushing), I recommend sipping fluids consistently throughout the day. This allows your body to absorb the fluid more efficiently and maintain a stable plasma volume.
2. The Electrolyte Boost
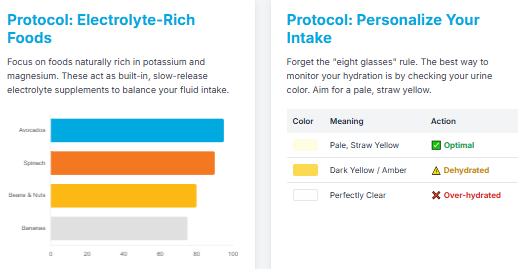
I actively incorporate natural electrolyte sources into my daily routine:
- Electrolyte Drink: I often start my day with a large glass of water that includes a pinch of high-quality sea salt (for sodium and trace minerals) and a squeeze of lemon or lime (for trace potassium).
- Mineral-Rich Foods: I focus on foods naturally rich in potassium and magnesium: bananas, avocados, spinach, beans, and nuts. These foods act as built-in, slow-release electrolyte supplements.
- Broth: A simple vegetable or bone broth is one of the most effective ways to replenish both fluid and salt after heavy sweating or activity.
3. Personalize Your Intake
Forget the universal “eight glasses” rule. I monitor my hydration by checking my urine color: it should be a pale, straw yellow. If it’s dark, I need more fluid. If it’s perfectly clear, I may be over-hydrating and diluting my electrolytes.
My Personal Advice as a Health Advocate
Before I understood this subtle mechanism, I was accidentally undermining my own health goals. I was active, I was eating well, but I was sweating out essential minerals and only replacing them with plain water. This left me in a constant state of mild dehydration that I now believe contributed to my occasional blood pressure spikes.
Since adopting the balanced hydration protocol—mindful sipping, adding electrolytes, and eating potassium-rich foods—I’ve noticed a significant difference, not just in my blood pressure readings, but in my energy levels and mental clarity. It’s a powerful reminder that sometimes the solution to a complex chronic problem is found in the most fundamental and often overlooked pillar of health.
FAQs (Frequently Asked Questions)
Can sugary sports drinks fix dehydration?
While they contain electrolytes, the excessive sugar content is highly inflammatory and negates the health benefits. Stick to unsweetened water, natural juices, or homemade electrolyte mixes.
How does caffeine affect hydration?
Caffeine is a mild diuretic, meaning it causes you to excrete more fluid. If you rely heavily on coffee, it’s even more crucial to actively replace those fluids and minerals throughout the day.
Does herbal tea count toward my fluid intake?
Yes. Unsweetened herbal teas, especially those without caffeine, are an excellent way to count toward your daily fluid intake while providing antioxidants.
Are all salts the same for electrolytes?
No. Highly processed table salt is often stripped of trace minerals. I prefer using unrefined sea salt or pink Himalayan salt, which retain trace minerals beneficial for electrolyte balance.
Conclusion
The link between dehydration and elevated blood pressure is a silent, but potent, threat. Your body is constantly fighting to maintain a perfect fluid balance, and even minor shortfalls force it into a survival mode that constricts your blood vessels and stresses your heart.
I urge you to move beyond simply drinking water. Embrace the understanding that true, restorative hydration requires balancing water intake with essential electrolytes. By making this simple, conscious choice to fuel your cells with the right blend of fluids and minerals, you can actively reduce your blood pressure and safeguard your long-term cardiovascular health.
Start monitoring your urine color and sprinkle a little sea salt into your water today. It’s the smallest step that yields the biggest reward.
Disclaimer: I am a health advocate and writer, not a medical doctor. The information in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician.
Sources:
Vasopressin and Hypertension: Popkin, B. M., D’Anci, K. E., & Rosenberg, I. H. (2010). Water, Hydration, and Health. Nutrition Reviews, 68(8), 439–458.
Electrolytes and Blood Pressure: Stone, M. S., et al. (2016). Changes in Dietary Calcium, Magnesium, and Potassium Intake and the Risk of All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Advances in Nutrition, 7(5), 999–1011.



